
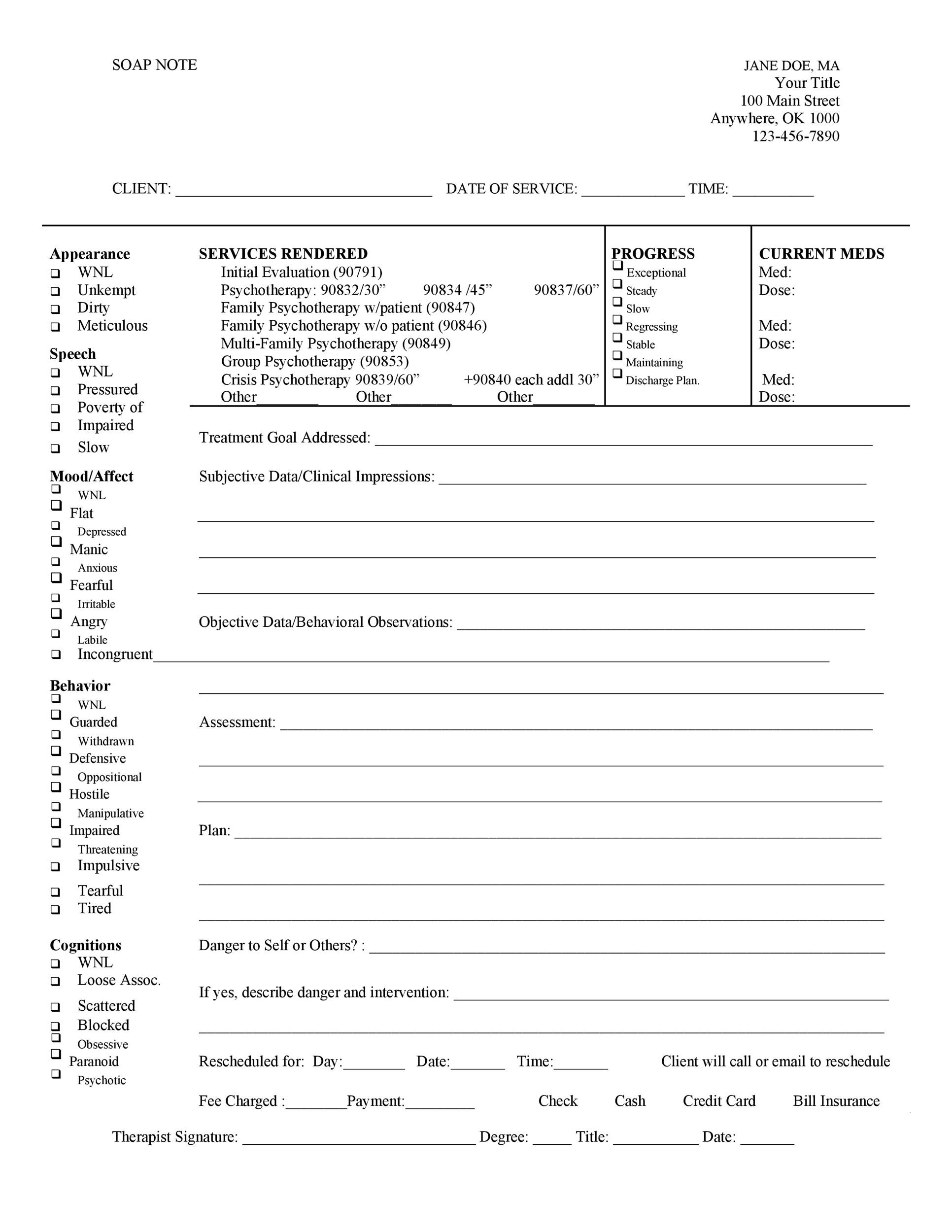
#SOAP NOTEA SOFTWARE#
The combined use of electronic health records and clinical note taking software has the potential to improve the overall quality of client care, increase efficiency of health practitioners, and reduce health care costs. Professional note taking and documentation is a skill and like any skill, it can be learned and improved.Ĭliniknote is designed by medical professionals to streamline and improve SOAP note taking Your documentation guides diagnosis, treatment, referral to other services and is a reflection of you and your profession. One of the most critical skills that allied health professionals must learn is effective documentation. SOAP notes should be accurate, easy to follow, access and share They are used in numerous health care settings to support a holistic approach to complex and wide ranging treatments for patients. In the past several years, electronic health records have also become the norm rather than the exception for healthcare providers. SOAP notes are now the most common method of documentation used by providers to input notes into patients’ medical records. Today it is not just doctors who interact with SOAP notes but also physiotherapists, occupational therapists, chiropractors, patients, billing and legal professionals, administrators and other health practitioners.
Īs part of a more patient-centric approach to documentation Weed recommended that the progress note be organised into four sections: Lawrence Weed, professor of medicine and pharmacology at Yale University who was inspired to create the basis of the SOAP note in the 1950’s to improve documentation and clinical reasoning in medicine. The recording of patient information has been traced back to cave paintings and stone carvings of prehistoric times and Egyptian surgical case reports documented on papyrus. Posted at 19:03h in Blogs by Jack Perisa 0 Comments


 0 kommentar(er)
0 kommentar(er)
